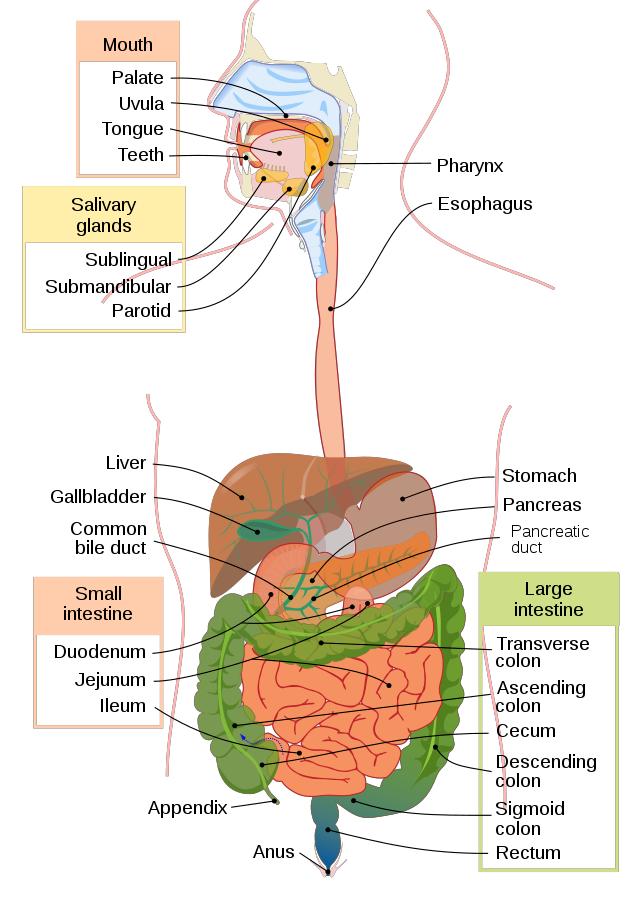
The gastrointestinal (GI) tract, also known as the digestive tract or alimentary canal (see the legend at the bottom of the page for the above image), is a long tube that runs from the mouth to the anus. It is responsible for the mechanical and chemical breakdown of food, and the absorption of nutrients and water. The main organs of the GI tract include the mouth, esophagus, stomach, small intestine, and large intestine. The pancreas, liver, and gallbladder also play important roles in the digestive process.
The process begins in the mouth, where food is broken down by enzymes and mechanically by the teeth and tongue. It then moves down the esophagus and into the stomach, where it is further broken down by stomach acid and enzymes. The small intestine is where most nutrient absorption takes place, and the large intestine primarily reabsorbs water and electrolytes and prepares waste for elimination.
From Upper to Lower:
The mouth is the first part of the alimentary canal, where food is taken in and mechanically broken down by the teeth and tongue. Salivary enzymes also begin the process of chemical breakdown. The food then moves down the esophagus, a muscular tube that propels the food to the stomach by a process called peristalsis.
The stomach is a muscular sac that mixes the food with stomach acid and enzymes to further break it down. The stomach also serves as a storage organ for food before it is moved on to the small intestine.
The small intestine is where most nutrient absorption takes place. The walls of the small intestine are lined with villi and microvilli which increase the surface area for absorption. The pancreas and liver secrete enzymes and bile into the small intestine to aid in digestion.
The large intestine (colon) is responsible for reabsorbing water and electrolytes and preparing waste for elimination. The feces are stored in the rectum until they are eliminated through the anus.
Discoveries:
Many scientists and physicians have made important contributions to our understanding of the digestive process over the centuries. Some of the major historical figures include:
- Andreas Vesalius (1514-1564): A Belgian anatomist and physician who made detailed observations of the structure of the human body, including the digestive system. He published a book called “De humani corporis fabrica” (On the Fabric of the Human Body), which was one of the first comprehensive works on human anatomy and included detailed illustrations of the digestive system.
- William Harvey (1578-1657): An English physician who was the first to describe the circulation of blood in the body. He also made important observations on the muscles of the digestive system and the role of the heart in the digestive process.
- Antoine Lavoisier (1743-1794): A French chemist and biologist who discovered that respiration and digestion were both forms of combustion and that they were both necessary for the maintenance of life. He also identified oxygen as a key component in the process of respiration.
- William Beaumont (1785-1853): An American physician who conducted a series of experiments on a patient with a fistula (an abnormal opening) in his stomach, which allowed Beaumont to observe the digestive process directly. Beaumont’s observations and experiments helped to establish the basic principles of gastric physiology and physiology of digestion.
- Ivan Pavlov (1849-1936): A Russian physiologist who is best known for his research on the digestive system, particularly the role of the salivary glands in the digestive process. He developed the concept of “conditioned reflexes,” which helped to explain how the body responds to different stimuli, including food.
- Roger Williams (1893-1988): an American biochemist who identified the presence of Vitamin B1 (thiamine) and Vitamin B3 (niacin) in the human diet. He also discovered a genetic disorder called pellagra which is caused by a deficiency of niacin.
- Sydney Ringer (1890-1956): an English physiologist who developed the Ringer solution, a saline solution that is still used today to maintain the physiological balance of fluids in the body during surgical procedures and other medical treatments.
- Albert Schatz (1920-2005): An American microbiologist who discovered the antibiotic streptomycin, which is effective against tuberculosis.
- Barry Marshall (born 1951): an Australian physician who, along with Robin Warren, discovered the bacterium Helicobacter pylori and its role in the development of gastritis and peptic ulcer disease.
- Andrew G. Burnham (born 1948): an American Physiologist and microbiologist who discovered that certain microorganisms that live in the human gut, such as Bacteroides thetaiotaomicron, can break down complex sugars that are resistant to digestion in the small intestine and upper colon, known as polysaccharides.
These are some of the major historical figures that contributed to the understanding of the digestive process, but there are many others who have made important contributions as well.
Common Disorders:
Common disorders of the digestive process include acid reflux, peptic ulcers, irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), celiac disease, and food poisoning. Other disorders include diverticulitis, gallstones, and pancreatitis.
Some of these conditions can be treated with medications, while others require more aggressive treatment, such as surgery. It is always best to consult a doctor for a proper diagnosis and treatment plan.
IBS:
There is ongoing research on irritable bowel syndrome (IBS), as it is a common condition that affects many people. Some recent studies have focused on identifying potential biomarkers for IBS, as well as investigating the effectiveness of various treatment options.
One recent study found that changes in gut bacteria may play a role in the development of IBS, and that probiotics may be a useful treatment for reducing symptoms.
Another study found that a low FODMAP diet, which is a diet that eliminates certain types of carbohydrates that can be difficult to digest, may be effective in reducing symptoms of IBS.
Research also suggests that psychological therapies such as cognitive-behavioral therapy and hypnotherapy may be effective in reducing symptoms of IBS.
Additionally, there is ongoing research in the field of gut-brain axis, which aims to understand the role of gut microbes and their interactions with the brain in IBS.
Acid Reflux:
Acid reflux, also known as gastroesophageal reflux disease (GERD), is a common condition in which stomach acid flows back into the esophagus, causing heartburn and other symptoms.
Recent research has focused on identifying potential causes of acid reflux and developing new treatment options. One study found that obesity and a high fat diet may contribute to the development of acid reflux.
Another study found that a Mediterranean diet, which is rich in fruits, vegetables, whole grains, and healthy fats, may be effective in reducing symptoms of acid reflux.
Research also suggests that certain lifestyle changes, such as avoiding trigger foods, losing weight, and avoiding eating late at night, can help to reduce symptoms of acid reflux.
Medications such as proton pump inhibitors (PPIs) and H2 receptor antagonists are the most common treatment for acid reflux, but research has also been conducted on other medications such as pro-motility agents, and even nerve stimulation.
Research is continuously being conducted and new findings and treatment options may become available in the future.
Peptic Ulcers:
Peptic ulcers are sores that form on the lining of the stomach and upper portion of the small intestine, known as the duodenum. They are caused by the erosion of the mucous membrane by stomach acid and pepsin.
Recent research has focused on identifying the causes of peptic ulcers and developing new treatment options. Historically, peptic ulcers were thought to be caused by stress and lifestyle factors such as diet, but it is now known that the majority of peptic ulcers are caused by a bacterial infection with H. pylori, and treated with antibiotics.
Recent studies have shown that treatment of H. pylori infection with a combination of antibiotics, as well as proton pump inhibitors (PPIs) and other acid-reducing medications, can be effective in healing peptic ulcers and preventing their recurrence.
Research has also been conducted on the use of new antibiotics, as well as new combination of drugs, to help eliminate H. pylori infection.
Additionally, research is also being done on the use of probiotics as a complementary treatment for peptic ulcers, as well as on new surgical options for patients who don’t respond to medical treatment.
Research is continuously being conducted and new findings and treatment options may become available in the future. It is always best to consult a healthcare professional for the most up-to-date information and treatment options.
Inflammatory bowel disease (IBD) is a term that refers to a group of chronic inflammatory conditions that affect the digestive tract, including Ulcerative Colitis (UC) and Crohn’s Disease (CD). These conditions are characterized by inflammation of the gastrointestinal tract, which can lead to symptoms such as abdominal pain, diarrhea, rectal bleeding, and weight loss.
Recent research on IBD has focused on identifying the causes of these conditions and developing new treatment options. It is believed that IBD is caused by a combination of genetic, environmental, and immune system factors.
Recent studies have shown that treatment with biologic drugs, such as anti-TNF therapies, can be effective in reducing inflammation and improving symptoms of IBD.
Research has also been conducted on the use of new biologic drugs, such as anti-integrin therapies, and immunomodulators, for the treatment of IBD.
Additionally, research is also being done on the use of probiotics as a complementary treatment for IBD, as well as new surgical options for patients who don’t respond to medical treatment.
There is also ongoing research on the gut-microbiome connection in IBD, with studies suggesting that changes in the gut microbiome may play a role in the development and progression of the disease.
Difference Between IBS and IBD:
Irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) are both conditions that affect the digestive system, but they are different in several key ways.
IBS is a functional disorder, which means that it is a condition that affects the way the muscles in the gut function, causing symptoms such as abdominal pain, bloating, and constipation or diarrhea. IBS does not cause inflammation or damage to the gut, and it is not a progressive disease.
IBD, on the other hand, is a group of chronic inflammatory conditions that affect the digestive tract, including Ulcerative Colitis and Crohn’s Disease. These conditions are characterized by inflammation of the gastrointestinal tract, which can lead to symptoms such as abdominal pain, diarrhea, rectal bleeding, and weight loss. IBD can cause permanent damage to the gut and increases the risk of colon cancer.
Another difference is that IBS is diagnosed based on symptoms and a physical exam, while IBD is diagnosed through a combination of blood tests, stool tests, imaging tests and a colonoscopy or endoscopy.
Treatment for IBS may include dietary changes, probiotics, and psychological therapies such as cognitive-behavioral therapy and hypnotherapy. Treatment for IBD typically includes medication such as anti-inflammatory drugs, immunomodulators, and biologic therapies, as well as surgery in some cases.
Celiac Disease:
Celiac disease is an autoimmune disorder that affects the digestive system. It is triggered by the consumption of gluten, which is a protein found in wheat, barley, and rye. When someone with celiac disease eats gluten, it causes an immune response in the small intestine, which leads to inflammation and damage to the lining of the gut. This can lead to a wide range of symptoms, including diarrhea, abdominal pain, and weight loss, as well as malabsorption of nutrients.
Recent research on celiac disease has focused on identifying the causes and risk factors of the disease, as well as developing new treatment options. Research has shown that celiac disease is caused by a combination of genetic and environmental factors. Studies have identified several genes that are associated with an increased risk of celiac disease, and research continues on understanding the genetics of the disease.
The only treatment for celiac disease is a gluten-free diet, which can be a significant lifestyle change and may be difficult to maintain. There are also ongoing research to develop new drugs that can be taken in addition to a gluten-free diet, to help reduce symptoms and inflammation in the gut.
Research also suggests that a gluten-free diet may not be enough for some people with celiac disease, as they may still have damage to their gut even if they are not consuming gluten.
Food Poisoning:
There are many different types of food poisoning, caused by a variety of different bacteria, viruses, and parasites. Here is a list of some of the ailments from least serious to more serious:
- Stomach flu (viral gastroenteritis): This is caused by a variety of viruses, such as norovirus and rotavirus. Symptoms include nausea, vomiting, diarrhea, and stomach cramps, but they tend to be relatively mild and short-lived.
- Salmonella infection: This is caused by the bacteria Salmonella and can be contracted by consuming contaminated food, such as raw or undercooked meat, eggs, or dairy products. Symptoms include diarrhea, fever, and abdominal cramps and usually last for 4-7 days.
- Campylobacter infection: This is caused by the bacteria Campylobacter and can be contracted by consuming contaminated food, such as raw or undercooked poultry or untreated water. Symptoms include diarrhea, cramping, and fever and usually last for 2-5 days.
- Listeria infection: This is caused by the bacteria Listeria and can be contracted by consuming contaminated food, such as deli meats, unpasteurized dairy products, and certain types of seafood. Symptoms include fever, muscle aches, and nausea, but in some cases, it can lead to serious complications such as meningitis.
- E. coli infection: This is caused by the bacteria Escherichia coli and can be contracted by consuming contaminated food, such as undercooked beef, raw milk, and untreated water. Symptoms include severe diarrhea and abdominal cramps, and in some cases, it can lead to kidney failure.
This list is not exhaustive, and there are other types of food poisoning that can be caused by other microorganisms. Also, some food poisoning can be more severe or cause more dangerous complications depending on the individual, specially in people with compromised immune systems, pregnant women and older adults.
It’s always best to take food safety precautions, such as washing your hands and food thoroughly, cooking meat to the appropriate temperature, and avoiding cross-contamination, to prevent food poisoning. If you suspect you have food poisoning, it’s important to seek medical attention right away.
Diverticulitis:
Diverticulitis is a condition in which small, bulging pouches (diverticula) that form in the lining of the large intestine become inflamed or infected.
Recent research on diverticulitis has focused on identifying the causes of the condition, as well as developing new treatment options.
One recent study found that a high-fiber diet may help to reduce the risk of diverticulitis. The study suggests that a diet high in fiber may help to prevent constipation and promote regular bowel movements, which may reduce the risk of diverticula forming in the first place.
Another study found that a low-residue diet may be more effective in managing symptoms of diverticulitis than a high-fiber diet.
Research also suggests that probiotics may be effective in reducing the risk of diverticulitis.
Additionally, research is also being done on the use of antibiotics in the treatment of diverticulitis, as well as new surgical options for patients who don’t respond to medical treatment.
Gallstones:
Gallstones are hard, pebble-like deposits that form in the gallbladder, a small organ located in the upper right portion of the abdomen. They can be as small as a grain of sand or as large as a golf ball, and they can be made up of cholesterol, bilirubin, or a combination of both.
Recent research on gallstones has focused on identifying the causes of the condition, as well as developing new treatment options.
Some studies have shown that a diet that is high in fat and cholesterol may increase the risk of developing gallstones.
Other studies have found that obesity, rapid weight loss, and certain medical conditions, such as diabetes, can also increase the risk of gallstones.
Research also suggests that certain medications, such as birth control pills and hormone replacement therapy, may increase the risk of gallstones.
There are several treatment options for gallstones, including medication, surgery, and lifestyle changes. Medications, such as ursodeoxycholic acid (UDCA) may be used to dissolve small gallstones and reduce symptoms, but they are not effective for larger gallstones. Surgery is the most common treatment for gallstones, which involves removal of the gallbladder (cholecystectomy) which is usually done laparoscopically.
Lifestyle changes such as maintaining a healthy weight, eating a balanced diet, and avoiding rapid weight loss can also help to prevent the formation of gallstones.
Pancreatitis:
Pancreatitis is a condition in which the pancreas, an organ located behind the stomach, becomes inflamed. Acute pancreatitis is a sudden onset of inflammation that can last for several days, while chronic pancreatitis is a long-term inflammation that can lead to permanent damage to the pancreas.
Recent research on pancreatitis has focused on identifying the causes of the condition, as well as developing new treatment options.
Some studies have found that alcohol abuse and gallstones are the most common causes of acute pancreatitis. Other causes include high triglycerides levels, certain medications, and certain medical conditions such as cystic fibrosis.
Research has also been conducted on the use of new medications, such as somatostatin analogs, for the treatment of acute pancreatitis.
Additionally, research is also being done on the use of probiotics as a complementary treatment for pancreatitis, as well as new surgical options for patients who don’t respond to medical treatment.
In the case of chronic pancreatitis, research has been directed in understanding the underlying mechanisms, such as the role of genetics and environmental factors, as well as developing new treatments options, such as stem cell therapy, enzyme replacement therapy and gene therapy.
Books:
- “Gastrointestinal and Liver Disease: Pathophysiology, Diagnosis, Management” by Mark Feldman, Lawrence S. Friedman, and Lawrence J. Brandt. This book is considered a classic in the field of gastrointestinal medicine and provides a comprehensive overview of the pathophysiology, diagnosis, and management of GI and liver disorders.
- “The Color Atlas of Internal Medicine” by Richard Usatine, Smitha Mundlapudi, and E. J. Mayeaux Jr. This book is a visual guide to the diagnosis and treatment of common internal medicine conditions, including gastrointestinal disorders. It contains over 1000 high-quality images and illustrations that help to clarify complex concepts.
- “Principles and Practice of Gastrointestinal Oncology” by James L. Abbruzzese and David Kelsen. This book is a comprehensive resource on the management of gastrointestinal malignancies, including esophageal, gastric, pancreatic, liver, and colorectal cancer. It covers the latest advances in the field, including new therapies, surgical techniques, and radiation therapies.
Research:
- “A randomized trial of aspirin to prevent colorectal adenomas” by Nancy R. Cook, Peter M. Rothwell, and J. Michael Gaziano. Published in the New England Journal of Medicine in 2010, this study found that daily low-dose aspirin reduced the incidence of colorectal adenomas, precursors to colorectal cancer, in a high-risk population.
- “The role of Helicobacter pylori in peptic ulcer disease” by Barry J. Marshall and J. Robin Warren. Published in the Lancet in 1984, this study proposed that the bacterium Helicobacter pylori is responsible for most peptic ulcers, challenging the long-held belief that stress and lifestyle factors were the primary causes of the condition.
- “Randomized trial of endoscopic versus open surgical drainage of walled-off pancreatic necrosis” by Sebastiaan J. H. Hulshof, Pieter Besselink, and Jan G. N. van Randen. Published in The Lancet in 2011, this study found that endoscopic drainage of walled-off pancreatic necrosis is a safe and effective alternative to open surgical drainage for the management of this condition. This study is widely cited in the field of gastrointestinal disorders and pancreatitis treatment.