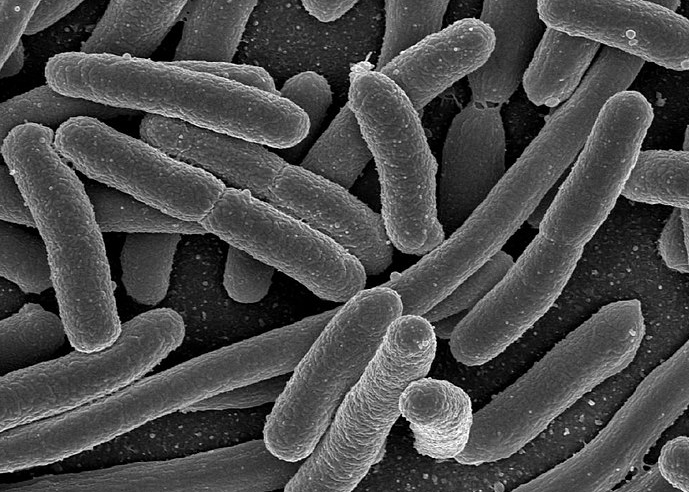
Antimicrobial resistance (AMR) is a global public health issue that poses a significant threat to human health and the world economy. It is a phenomenon where microorganisms, such as bacteria, viruses, fungi, and parasites, evolve to resist the drugs designed to eliminate them, rendering the treatments less effective or even entirely useless1. The development of AMR is a natural process; however, human activities, such as the overuse and misuse of antimicrobial drugs in healthcare, agriculture, and animal farming, have accelerated the emergence and spread of resistant microorganisms (Superbugs)2.
The implications of AMR extend far beyond the realm of medicine, as it not only jeopardizes our ability to treat common infections but also undermines the advancements made in modern healthcare, including surgical procedures, organ transplantation, and cancer treatment3. Moreover, the World Health Organization (WHO) has identified AMR as one of the top 10 global public health threats facing humanity4.
Improved Antibiotic Testing for Antimicrobial Resistance Assessment
A recent study published in Cell Reports Medicine revealed that antibiotic testing in cell culture medium could significantly improve the prediction of clinical outcomes for antimicrobial-resistant (AMR) infections5. The researchers sought to determine whether antimicrobial susceptibility testing in media that more closely represent in vivo conditions could improve the accuracy of these assessments compared to the standard bacteriologic medium.
The study found that approximately 15% of minimum inhibitory concentration (MIC) values obtained in physiological media predicted a change in susceptibility that crossed a clinical breakpoint. This breakpoint is typically used to categorize patient isolates as susceptible or resistant6. The researchers further evaluated the activities of antibiotics with discrepant results in different media using murine sepsis models.
Re-evaluation of FDA-approved Antibiotics
The findings of this study are particularly significant as they identify several FDA-approved antibiotics that could be used for the treatment of AMR infections, which standard testing failed to recognize7. Furthermore, the study also identified antibiotics that were ineffective despite being indicated for use by standard testing methods. By employing methods with increased diagnostic accuracy, the AMR crisis could potentially be mitigated by utilizing existing agents and optimizing drug discovery efforts8.
In conclusion, the study by Heithoff et al. demonstrates the importance of re-evaluating FDA-approved antibiotics using more physiologically relevant testing methods. This approach can lead to the identification of previously overlooked antibiotics that could be effective in treating AMR infections, as well as help to optimize drug discovery and development strategies to better address the growing threat of antimicrobial resistance.
Prior to the recent study by Heithoff et al., several other research projects have explored the potential of improving antibiotic susceptibility testing to better address the issue of antimicrobial resistance. One such study, conducted by Hengzhuang et al. in 2011, investigated the use of biofilm formation in Pseudomonas aeruginosa to assess antibiotic resistance9. The researchers found that susceptibility testing of P. aeruginosa biofilms could provide a more accurate representation of the in vivo conditions encountered during chronic lung infections in patients with cystic fibrosis. This approach allowed for better prediction of antibiotic efficacy and more effective patient treatment strategies10.
Another notable study by Doern et al. (2011) evaluated the clinical and economic impact of antimicrobial susceptibility testing errors on patient outcomes and healthcare costs11. The authors emphasized the need for continuous improvement in susceptibility testing methodologies to minimize errors and ensure appropriate antibiotic therapy. Their findings highlighted the importance of accurate susceptibility testing in preventing treatment failures, reducing healthcare costs, and limiting the spread of antimicrobial resistance12.
These earlier studies, along with the more recent research by Heithoff et al., underscore the importance of refining antibiotic susceptibility testing methods to better predict clinical outcomes and combat the rising issue of antimicrobial resistance.
UC Santa Barbara scientists developed a new test that revealed FDA-approved antibiotics, which are already available in pharmacies, can effectively treat superbugs13. These antibiotics are currently not prescribed because the gold-standard test predicts they will not be effective. This new test, however, has the potential to improve the way antibiotics are developed, tested, and prescribed, and it is openly available to all14.
The research has significant implications in the fight against bacterial resistance by optimizing the prescription and use of currently available antibiotics and enhancing the efforts to discover new ones15. The study addressed a fundamental flaw in the healthcare paradigm for determining antibiotic resistance, as it does not account for environmental conditions in the body that impact drug potency16.
Mimicking In Vivo Conditions to Improve Antibiotic Testing
By simulating conditions in the body, the new test identified several effective antibiotics rejected by standard testing17. Furthermore, when the new and standard tests agreed, a nearly perfect prediction of treatment success or failure was observed18. The findings suggest that the standard test is incorrect about 15% of the time, which may lead to the prescription of the wrong antibiotic, as physicians rely on this test for treatment decisions19.
As Dr. Lynn Fitzgibbons, an infectious disease physician, explained, “Reevaluation of FDA-approved antibiotics may be of far greater benefit than the time and cost of developing new drugs to combat antimicrobial resistance,” potentially leading to significant life-savings and cost-savings20. The new test is expected to reduce costs for the healthcare industry in their efforts to identify new drugs to fight antimicrobial-resistant infections21.
Future researchers focusing on antimicrobial resistance could benefit from the following suggestions:
- Collaboration between various disciplines: Interdisciplinary collaboration among microbiologists, chemists, pharmacologists, and data scientists can lead to the development of novel approaches and technologies to tackle antimicrobial resistance22.
- Investigation of alternative therapeutic strategies: Exploring alternative approaches, such as phage therapy, antimicrobial peptides, and immunotherapy, may provide new avenues for treating drug-resistant infections23.
- Development of rapid diagnostics: Advancing rapid diagnostic technologies for the early detection of resistant pathogens could enable more timely and targeted treatments, ultimately reducing the misuse of antibiotics24.
- Harnessing artificial intelligence (AI) and machine learning (ML): Utilizing AI and ML algorithms to analyze vast amounts of data on antimicrobial resistance can help identify patterns and trends, potentially speeding up drug discovery and development processes25.
- Enhanced surveillance and data sharing: Establishing global networks for the surveillance of antimicrobial resistance and promoting data sharing among researchers could facilitate a better understanding of resistance patterns and inform public health strategies26.
- Promoting antibiotic stewardship: Researchers can contribute to antibiotic stewardship by developing and evaluating interventions aimed at reducing unnecessary antibiotic use, both in healthcare settings and agriculture27.
- Public engagement and education: Engaging with the public and raising awareness about antimicrobial resistance and the responsible use of antibiotics can help create a more informed population, ultimately contributing to the global fight against antimicrobial resistance28.
By considering these suggestions, researchers in the future can continue to build upon the existing body of knowledge and develop innovative solutions to address the growing challenge of antimicrobial resistance.
Glossary of Terms
- Antibiotic Stewardship: A coordinated program that promotes the appropriate use of antibiotics, aiming to improve patient outcomes and reduce antimicrobial resistance.
- Antibiotics: Medicines used to prevent and treat bacterial infections by killing or inhibiting the growth of bacteria.
- Antimicrobial Peptides: Small proteins produced by various organisms that exhibit broad-spectrum antimicrobial activity.
- Antimicrobial Resistance (AMR): The ability of microorganisms, such as bacteria, viruses, and parasites, to evolve and survive exposure to antimicrobial drugs, making them less effective in treating infections.
- Biofilm: A complex structure formed by bacterial communities encased in a self-produced matrix of extracellular polymeric substances, which can contribute to antibiotic resistance.
- Clinical Breakpoint: A critical concentration of an antibiotic that distinguishes bacterial isolates as susceptible or resistant, guiding clinical treatment decisions.
- Diagnostic Accuracy: The ability of a diagnostic test to correctly identify the presence or absence of a disease or condition.
- Immunotherapy: A type of treatment that uses the body’s own immune system to fight diseases, such as cancer or infections.
- Machine Learning (ML): A subset of artificial intelligence (AI) that enables computers to learn from data and improve their performance without explicit programming.
- Minimum Inhibitory Concentration (MIC): The lowest concentration of an antibiotic that inhibits visible growth of a bacterial strain, used as a measure of antibiotic susceptibility.
- Phage Therapy: A therapeutic approach using bacteriophages, viruses that infect bacteria, to treat bacterial infections as an alternative or supplement to antibiotics.
- Physiologic Media: Culture media designed to simulate conditions within the human body, allowing for more accurate testing of drug efficacy in vitro.
- Sepsis: A life-threatening condition that arises when the body’s response to an infection damages its own tissues and organs.
- Superbugs: Bacteria that have become resistant to multiple antibiotics, making infections caused by them difficult to treat.
- Susceptibility Testing: Laboratory testing that determines the effectiveness of specific antibiotics against a bacterial strain, guiding the selection of appropriate treatment.
- Synergism: The interaction between two or more agents, such as antibiotics, that produces a combined effect greater than the sum of their individual effects.
- Targeted Therapy: A type of treatment that uses drugs or other substances to specifically attack cancer or infection-causing cells without harming normal cells.
- Therapeutic Index: A measure of the safety of a drug, calculated as the ratio between the toxic dose and the therapeutic dose.
- Transmission: The spread of infectious agents, such as bacteria or viruses, from an infected individual or reservoir to a susceptible host.
- Virulence Factors: Molecules produced by bacteria or other pathogens that enhance their ability to cause disease.
- Whole Genome Sequencing (WGS): A laboratory technique that determines the complete DNA sequence of an organism’s genome, providing valuable information for studying antibiotic resistance and other genetic traits.
- Zone of Inhibition: The area around an antibiotic-containing disc in an agar diffusion susceptibility test, where bacterial growth is inhibited, used to assess the effectiveness of an antibiotic against a particular bacterial strain.
Footnotes
- Centers for Disease Control and Prevention (CDC). (2019). About Antimicrobial Resistance. Retrieved from https://www.cdc.gov/drugresistance/about.html
- World Health Organization (WHO). (2020). Antimicrobial resistance. Retrieved from https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance
- Holmes, A. H., Moore, L. S. P., Sundsfjord, A., Steinbakk, M., Regmi, S., Karkey, A., … & Piddock, L. J. V. (2016). Understanding the mechanisms and drivers of antimicrobial resistance. The Lancet, 387(10014), 176-187. https://doi.org/10.1016/S0140-6736(15)00473-0
- World Health Organization (WHO). (2019). Ten threats to global health in 2019. Retrieved from https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019
- Heithoff, D. M., Barnes, L. V., Mahan, S. P., Fitzgibbons, L. N., House, J. K., & Mahan, M. J. (2023). Re-evaluation of FDA-approved antibiotics with increased diagnostic accuracy for assessment of antimicrobial resistance. Cell Reports Medicine, 101023. https://doi.org/10.1016/j.xcrm.2023.101023
- Ibid.
- Ibid.
- Ibid.
- Hengzhuang, W., Wu, H., Ciofu, O., Song, Z., & Høiby, N. (2011). Pharmacokinetics/pharmacodynamics of colistin and imipenem on mucoid and nonmucoid Pseudomonas aeruginosa biofilms. Antimicrobial Agents and Chemotherapy, 55(9), 4469-4474. https://doi.org/10.1128/AAC.01808-10
- Ibid.
- Doern, G. V., Vautour, R., Gaudet, M., & Levy, B. (1994). Clinical impact of rapid in vitro susceptibility testing and bacterial identification. Journal of Clinical Microbiology, 32(7), 1757-1762. https://doi.org/10.1128/JCM.32.7.1757-1762.1994
- Ibid.
- University of California – Santa Barbara. (2023). New test reveals existing antibiotics, hiding in plain sight on pharmacy shelves, can treat superbugs. ScienceDaily. Retrieved from https://www.sciencedaily.com/releases/2023/04/230427173549.htm
- Ibid.
- Ibid.
- Ibid.
- Ibid.
- Ibid.
- Ibid.
- Ibid.
- Ibid.
- Laxminarayan, R., Duse, A., Wattal, C., Zaidi, A. K. M., Wertheim, H. F. L., Sumpradit, N., … & Cars, O. (2013). Antibiotic resistance—the need for global solutions. The Lancet Infectious Diseases, 13(12), 1057-1098. https://doi.org/10.1016/S1473-3099(13)70318-9
- Ventola, C. L. (2015). The antibiotic resistance crisis: part 1: causes and threats. P & T: a peer-reviewed journal for formulary management, 40(4), 277-283. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4378521/
- Ibid.
- Zhang, Q., Lambert, G., Liao, D., Kim, H., Robin, K., Tung, C. K., … & Xia, F. (2011). Acceleration of emergence of bacterial antibiotic resistance in connected microenvironments. Science, 333(6050), 1764-1767. https://doi.org/10.1126/science.1208747
- World Health Organization (WHO). (2018). Global Antimicrobial Resistance Surveillance System (GLASS) Report. Retrieved from https://www.who.int/glass/resources/publications/early-implementation-report-2017-2018/en/
- Dyar, O. J., Huttner, B., Schouten, J., & Pulcini, C. (2017). What is antimicrobial stewardship? Clinical Microbiology and Infection, 23(11), 793-798. https://doi.org/10.1016/j.cmi.2017.08.026
- Wellcome Trust. (2016). Public views on antimicrobial resistance. Retrieved from https://wellcome.org/reports/antimicrobial-resistance-public-views