| Listen to our audio presentation: Managing Diabetes |
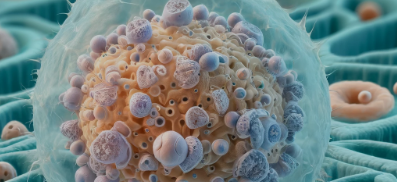
Batten disease, primarily affecting children, manifests as a fatal neurodegenerative disorder stemming from mutations in the CLN3 gene. Recent research published in Cell provides groundbreaking insights into the molecular dynamics of this disease, focusing on the role of glycerophosphodiesters (GPDs) in lysosomal phospholipid metabolism disruption.
Accumulation of GPDs in CLN3 Deficiency: Researchers found that loss of CLN3, a lysosomal protein, leads to an overwhelming buildup of GPDs in lysosomes. These compounds, derived from the breakdown of glycerophospholipids, interfere with the normal functioning of lysosomes, vital for cellular waste management.
Phospholipase Inhibition by GPDs: GPDs were identified as potent inhibitors of key lysosomal phospholipases, namely PLA2G15 and PLBD2. These enzymes, crucial for phospholipid catabolism, are hindered in their function, culminating in the accumulation of neurotoxic lysophospholipids.
Mechanistic Insights and Therapeutic Avenues: The study elucidates the mechanistic pathway of GPD-mediated inhibition of phospholipase activity, paving the way for novel therapeutic strategies targeting GPD clearance to alleviate Batten disease symptoms.
Batten disease is a subset of lysosomal storage disorders (LSDs) typified by the buildup of waste material in cell organelles called lysosomes. Understanding the role of GPDs in Batten disease provides not only insights into this specific condition but also broadens our comprehension of LSDs in general. The detailed characterization of PLA2G15 and PLBD2 enzymes sheds light on lysosomal lipid metabolism, potentially offering new targets for therapeutic intervention across various LSDs.
History of Batten Disease Discovery
Batten disease, part of a group of disorders known as neuronal ceroid lipofuscinoses (NCLs), was first described over a century ago. Here is a brief history:
1903: The first known description of Batten disease was made by Dr. Frederick Batten in London. He observed a peculiar form of neurodegeneration in two siblings, noting the progressive nature of vision loss, seizures, and cognitive decline.
1914: Dr. Heinrich Vogt further detailed the clinical spectrum of the disease, noting the presence of certain ocular symptoms and progressive neurological deterioration. The terms “Batten disease” and “Spielmeyer-Vogt disease” were initially used to describe the juvenile form of NCL.
1960s-1970s: With the advent of electron microscopy, researchers identified the ultrastructural hallmark of NCLs: the accumulation of autofluorescent lipopigments in neurons and other cell types, resembling ceroid and lipofuscin.
1990s: Advances in molecular genetics led to the identification of the first genes associated with NCL, marking a significant leap in understanding the disease’s genetic basis. The CLN3 gene, associated with the juvenile form of NCL, was among the first to be identified.
21st Century: To date, mutations in at least 14 different genes (CLN1 to CLN14) have been linked to various forms of NCLs, signifying the genetic and clinical heterogeneity of Batten disease.
Glossary of Terms
- Batten Disease/Neuronal Ceroid Lipofuscinosis (NCL): A group of rare, fatal, inherited disorders of the nervous system that usually manifest in childhood, characterized by the accumulation of lipopigments in the body’s tissues.
- CLN3 Gene: A gene whose mutations are most commonly associated with the juvenile form of Batten disease, leading to lysosomal dysfunction.
- Glycerophosphodiesters (GPDs): Metabolic products from the breakdown of glycerophospholipids, implicated in the pathology of Batten disease due to their accumulation in lysosomes.
- Lysosome: A cell organelle that digests and processes molecules to clear cellular waste.
- Phospholipase: An enzyme that breaks down phospholipids into fatty acids and other lipophilic substances.
- PLA2G15 and PLBD2: Specific types of lysosomal phospholipases implicated in the pathology of Batten disease due to their inhibition by accumulated GPDs.
- Lysophospholipids: Derivatives of phospholipids, known to be toxic and accumulate in lysosomes in the context of Batten disease.
- Neurodegeneration: The progressive loss of structure or function of neurons, including death of neurons, leading to diseases like Batten disease.
- Lipofuscin: A complex lipid-containing residue of lysosomal digestion, the accumulation of which is a hallmark of Batten disease and other NCLs.
- Ceroid: Autofluorescent lipopigment with similarities to lipofuscin, accumulating in cells and tissues in NCLs.
- Autofluorescent: Having the ability to emit light upon stimulation by a light source, characteristic of substances like ceroid and lipofuscin in NCLs.
Diseases Confused with Batten Disease
Batten disease, due to its neurological symptoms and progressive nature, can be confused with other neurodegenerative disorders, especially in the early stages. Here are some conditions with overlapping symptoms:
- Alzheimer’s Disease: Although typically affecting older adults, early-onset forms can present symptoms similar to Batten disease, like cognitive decline and memory loss.
- Parkinson’s Disease: Shares movement-related symptoms with Batten, such as tremors and rigidity, but usually occurs in older adults.
- Huntington’s Disease: Characterized by movement disorders, cognitive decline, and psychiatric symptoms, resembling late-stage Batten disease.
- Juvenile Amyotrophic Lateral Sclerosis (ALS): While ALS primarily affects motor neurons, its juvenile form can mimic Batten disease due to progressive muscle weakness and neurodegeneration.
- Friedreich’s Ataxia: This genetic disease causes progressive damage to the nervous system, resulting in symptoms like speech problems and coordination difficulties that are also seen in Batten disease.
- Epilepsy: Given that seizures are a common symptom in Batten disease, it can be initially mistaken for epilepsy disorders, especially those with progressive cognitive and motor decline.
Treatments for Batten Disease
As of now, there is no cure for Batten disease, but treatments are available to help manage symptoms and improve quality of life. Treatment options include:
- Enzyme Replacement Therapy (ERT): For some forms of NCL, ERT can be used to replace missing or deficient enzymes. For example, cerliponase alfa (Brineura) is approved for the treatment of CLN2 disease, a specific type of Batten disease.
- Gene Therapy: This experimental approach involves delivering a functional copy of the defective gene to cells. Clinical trials are underway to assess its efficacy in treating Batten disease.
Medications: Antiepileptic drugs are commonly prescribed to manage seizures, a primary symptom of Batten disease. Other medications may be used to address symptoms like spasticity, sleep disturbances, and psychiatric conditions. - Physical and Occupational Therapy: These therapies aim to maintain mobility and function, helping patients manage daily activities and maintain independence for as long as possible.
- Nutritional Support: Managing nutritional needs is crucial, as swallowing difficulties can arise. Speech therapists and dietitians can assist in creating feeding plans that ensure proper nutrition.
- Palliative Care: As Batten disease progresses, palliative care becomes essential to manage pain, provide comfort, and support both the patient and the family through the advanced stages of the disease.
- Management of Batten disease is multidisciplinary, involving neurologists, geneticists, nutritionists, physical and occupational therapists, and palliative care specialists to provide comprehensive care tailored to the individual’s needs.
Resources:
Mole, Sara, Ruth Williams, and Hans Goebel (eds), The Neuronal Ceroid Lipofuscinoses (Batten Disease), 2 edn, Contemporary Neurology Series (Oxford, 2011; online edn, Oxford Academic, 1 Nov. 2012), https://doi.org/10.1093/med/9780199590018.001.0001, accessed 5 Apr. 2024.
Glycerophosphodiesters inhibit lysosomal phospholipid catabolism in Batten disease Author: Kwamina Nyame,Andy Hims,Aya Aburous,Nouf N. Laqtom,Wentao Dong,Uche N. Medoh,Julia C. Heiby,Jian Xiong,Alessandro Ori,Monther Abu-Remaileh Publication: Molecular Cell Publisher: Elsevier Date: 4 April 2024
Diseases Similar to Batten Disease:
Mole, S. E., Williams, R. E., & Goebel, H. H. (2005). The Neuronal Ceroid Lipofuscinoses (Batten Disease). Oxford University Press. This book provides comprehensive information on Batten disease and its differential diagnosis with other neurodegenerative diseases.
Nardocci, N., Zorzi, G., Farina, L., et al. (2009). Progressive neurodegenerative disorders of childhood: Clinical and genetic overview. Neurol Sci, 30(3), 217-228. This review article discusses various progressive neurodegenerative disorders, including Batten disease, and highlights the clinical overlap with other conditions.
Treatments for Batten Disease:
Mink, J. W., Augustine, E. F., Adams, H. R., Marshall, F. J., & Kwon, J. M. (2013). Classification and natural history of the neuronal ceroid lipofuscinoses. Journal of Child Neurology, 28(9), 1101-1105. This paper discusses the classification and progression of NCLs and touches on treatment approaches.
Schulz, A., Ajayi, T., Specchio, N., et al. (2018). Study of Intraventricular Cerliponase Alfa for CLN2 Disease. New England Journal of Medicine, 378, 1898-1907. This study discusses the use of enzyme replacement therapy in treating a specific form of Batten disease.