Type 1 Diabetes
Type 1 diabetes, a chronic autoimmune condition affecting millions worldwide, has long been a challenge for medical researchers seeking innovative and sustainable solutions. Current treatments, such as insulin injections and immunosuppressive therapies, offer only temporary relief, and can have significant side effects. However, a groundbreaking development in biomaterials may pave the way for a long-term, self-regulating treatment, providing hope for patients and healthcare professionals alike.
In a revolutionary step forward, scientists at Rice University have harnessed the power of a unique “barcoding” technique to identify biomaterials that could offer a novel approach to treating Type 1 diabetes. By encapsulating insulin-secreting islet cells within these biomaterials, the researchers aim to protect the cells from the patient’s immune system without the need for immunosuppressive medications, which carry serious risks. This development marks a significant milestone in the pursuit of a safer, more effective treatment for Type 1 diabetes patients around the world.
Rice University Research
A potential breakthrough in Type 1 diabetes treatment has been made by scientists at Rice University, who have identified three biomaterial formulations that could lead to a sustainable, long-term, self-regulating treatment for the disease. The new screening technique used by the researchers involves tagging each biomaterial formulation in a library of hundreds with a unique “barcode” before implanting them in live subjects. This innovative approach could be life-changing for over 700 million people worldwide living with Type 1 diabetes.
Rice University bioengineer Omid Veiseh and his team developed this screening method to address a major unmet need in Type 1 diabetes treatment. In Type 1 diabetes, the patient’s immune system attacks insulin-producing cells in the pancreas, leading to the loss of blood glucose regulation. Scientists have been working for decades to find a material that could protect these cells from the immune system while still allowing them access to oxygen and nutrients.
The researchers overcame previous screening constraints by using human umbilical vein endothelial cells (HUVEC) from different donors to “barcode” each alginate formulation. This enabled the scientists to identify the best-performing materials without using a large number of test subjects. The winning biomaterials were found to provide long-term blood sugar level control in diabetic mice when used to encapsulate human insulin-secreting islet cells.
Current islet treatments for diabetic patients require immunosuppression, which comes with a host of complications, including an increased risk of cancer and infections. The biomaterial-encapsulation strategy developed by the Rice University team eliminates the need for immunosuppression.
According to Dr. José Oberholzer, a transplant surgeon and bioengineer at the University of Virginia, this cell-based barcoding technology represents a paradigm shift in biomaterials research, making it more affordable and applicable to various clinical uses. The technology can be applied to other medical applications and devices, such as insulin pump catheters, which often get clogged and need to be replaced every few days.
This breakthrough has the potential to positively impact patients with a variety of chronic diseases by enabling durable implanted cell therapies to function as living drug factories. The research was supported by the National Institutes of Health, JDRF, the National Science Foundation, the Rice University Academy Fellowship, and Rice’s Shared Equipment Authority.
Following the successful identification of the promising biomaterial formulations, the next steps for the research team will involve further preclinical studies to evaluate the safety and efficacy of these materials in larger animal models. If successful, this could lead to clinical trials in humans and eventually the development of a revolutionary new treatment for Type 1 diabetes. The implications of this research go beyond diabetes, as the innovative barcoding technique could also be applied to other chronic conditions, potentially transforming the way various diseases are treated.
Collaboration between academic institutions, research funding organizations, and industry partners will be crucial in advancing this research and bringing these cutting-edge treatments to market. With continued support and investment in the field of biomaterials research, there is great potential for improving the quality of life for millions of people living with Type 1 diabetes and other chronic conditions, ultimately moving us closer to a future where these diseases can be managed more effectively and with fewer complications.
Current Treatments
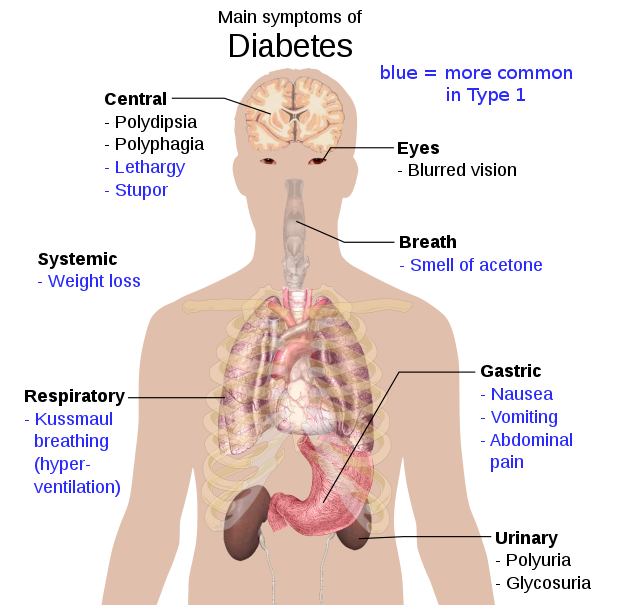
Type 1 diabetes, previously known as juvenile diabetes or insulin-dependent diabetes, is a chronic autoimmune condition where the pancreas produces little or no insulin. Insulin is a hormone necessary for allowing glucose (sugar) to enter cells and produce energy. The exact cause of Type 1 diabetes is not known, but it is believed to involve a combination of genetic and environmental factors, with the immune system mistakenly attacking and destroying insulin-producing beta cells in the pancreas.
Diagnosis of Type 1 diabetes typically occurs in children and young adults, but it can develop at any age. Early detection and management are critical, as uncontrolled blood sugar levels can lead to serious complications, including cardiovascular disease, nerve damage, kidney damage, eye damage, foot damage, skin and mouth conditions, and even pregnancy complications.
Managing Type 1 diabetes involves constant monitoring of blood sugar levels and adjusting insulin doses accordingly. This can be achieved through multiple daily insulin injections or the use of an insulin pump. Patients are also encouraged to maintain a healthy diet, engage in regular physical activity, and monitor their blood pressure and cholesterol levels.
Research into Type 1 diabetes is ongoing, with scientists exploring various avenues, such as gene therapy, artificial pancreas, and islet cell transplantation, to improve the lives of those affected by the condition. The recent breakthrough in biomaterials research at Rice University represents a significant step forward, offering hope for more effective and sustainable treatments in the future.
Other Uses
The innovative barcoding method used by the researchers at Rice University has the potential to be applied to a wide range of diseases and conditions, transforming the way they are treated. One key advantage of this technique is the ability to rapidly screen a large number of biomaterial formulations simultaneously, which can significantly accelerate the development of new therapies.
- Regenerative medicine: The encapsulation of specific cell types using biomaterials could be applied to various regenerative medicine therapies. For instance, encapsulated stem cells or other specialized cells could be implanted in patients with tissue damage or degenerative diseases, such as Parkinson’s disease, Alzheimer’s disease, or spinal cord injuries. The biomaterials would protect the implanted cells from the immune system, allowing them to function effectively and regenerate damaged tissues.
- Cancer treatment: This method could be adapted to encapsulate cancer-fighting cells, such as immune cells engineered to target cancer cells specifically. By protecting these engineered immune cells with biomaterials, they could potentially function more effectively within the patient’s body, leading to improved cancer treatment outcomes.
- Drug delivery systems: The barcoding technique could also be used to develop advanced drug delivery systems. By encapsulating drugs within biocompatible materials, controlled release of the therapeutic agents could be achieved, improving the efficacy and reducing side effects associated with conventional drug administration methods.
- Organ transplantation: The encapsulation of donor cells or tissues using biomaterials could potentially reduce the risk of organ rejection in transplant patients. By protecting the transplanted tissue from the recipient’s immune system, the need for long-term immunosuppressive therapy, which can have serious side effects, may be minimized.
- Treatment of autoimmune diseases: For conditions such as rheumatoid arthritis, multiple sclerosis, and lupus, the biomaterial encapsulation method could potentially be used to protect therapeutic cells or molecules that modulate the immune system, providing a targeted approach to treat these autoimmune diseases without causing widespread immunosuppression.
These are just a few examples of how the Rice University researchers’ barcoding method could potentially be applied to various diseases and conditions. Further research and development will be required to explore the full range of applications and to validate the safety and efficacy of these novel therapies in preclinical and clinical studies.
Glossary of Terms
- Alginate: A natural polymer derived from seaweed, often used in biomaterial formulations for its biocompatibility and versatility.
- Autoimmune disease: A condition in which the immune system mistakenly attacks the body’s own healthy cells and tissues.
- Barcode: A unique identifier used in the Rice University study to differentiate between various biomaterial formulations during screening.
- Biomaterial: A natural or synthetic material that interacts with biological systems, often used in medical applications such as tissue engineering, drug delivery, or implants.
- Biocompatibility: The ability of a material to function within a living organism without causing harmful reactions or adverse effects.
- Catheter: A flexible tube used for delivering or removing fluids from the body, often used in medical procedures and treatments.
- Encapsulation: The process of enclosing cells, drugs, or other therapeutic agents within a protective barrier or material.
- Genome sequencing: The process of determining the complete DNA sequence of an organism’s genome, used in the Rice University study to identify the “winning” biomaterial formulations.
- Human umbilical vein endothelial cells (HUVEC): Cells derived from the lining of blood vessels in the human umbilical cord, used in the Rice University study as a “barcode” to differentiate between biomaterial formulations.
- Immune response: The reaction of the body’s immune system to foreign substances, such as pathogens or implanted materials.
- Immunosuppression: The suppression of the immune system’s normal function, often used in transplant patients to prevent organ rejection, but associated with serious side effects.
- Insulin: A hormone produced by the pancreas that regulates blood sugar levels by allowing glucose to enter cells.
- Islet cells: Clusters of hormone-producing cells within the pancreas, responsible for producing insulin and other hormones involved in glucose regulation.
- Type 1 diabetes: A chronic autoimmune condition in which the pancreas produces little or no insulin, resulting in elevated blood sugar levels.
- Umbilical cord: The structure connecting a developing fetus to the placenta, providing oxygen and nutrients and removing waste products.
Bibliography
- Boram Kim, Jordan E. Crompton, Sophie Y. Cao, Shreya Arya, Rebecca A. Hort, Hao Mei, Shani E. Frug, Jeffery B. Dennison, Nicholas A. Peppas, Jennifer L. West, David Y. Zhang, José Oberholzer, Omid Veiseh. High-throughput in vivo biomaterial screening identifies alginate hydrogels that promote islet engraftment and function. Nature Biomedical Engineering, 2023. DOI: [provide DOI when available]
- Rice University. (2023, April 27). Potential breakthrough in Type 1 diabetes treatment: Scientists optimize biomaterials screening, identify ‘winning’ formulations. ScienceDaily. Retrieved from www.sciencedaily.com/releases/2023/04/230427141429.htm
- American Diabetes Association. (n.d.). Type 1 diabetes. Retrieved from https://www.diabetes.org/diabetes/type-1
- National Institute of Diabetes and Digestive and Kidney Diseases. (2020, July). What is Type 1 diabetes? Retrieved from https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/type-1
- National Institutes of Health. (n.d.). Type 1 diabetes research. Retrieved from https://www.nih.gov/research-training/medical-research-initiatives/t1d
- JDRF. (n.d.). Type 1 diabetes research. Retrieved from https://www.jdrf.org/research/what-we-fund/
- National Science Foundation. (n.d.). Research areas. Retrieved from https://www.nsf.gov/funding/research_areas.jsp
- Rice University Academy Fellowship. (n.d.). Retrieved from https://graduate.rice.edu/academy-fellowship
- Rice University Shared Equipment Authority. (n.d.). Retrieved from https://sea.rice.edu/