Abnormal RNA splicing is increasingly recognized as an important driver of many human diseases, including cancer. A new study led by researchers at Weill Cornell Medicine demonstrates the power of analyzing RNA splicing patterns in individual cells to elucidate how mutations disrupt normal gene regulation and contribute to disease. Using an enhanced single-cell multi-omics technique called GoT-Splice, the researchers profiled splicing alterations in bone marrow cells from patients with a myelodysplastic syndrome caused by mutations in the splicing factor SF3B1.
Their analysis provides unprecedented insight into how this mutation tilts cell maturation toward the red blood cell lineage, causes characteristic abnormalities in immature red cells, and allows mutation-containing cells to proliferate abnormally. The findings illuminate the mechanisms by which splicing factor mutations promote myelodysplastic syndrome and identify potential therapeutic targets, such as the apoptosis regulator BAX.
More broadly, this work establishes a powerful new tool for connecting splicing alterations to disease phenotypes at single-cell resolution across cell types and stages of differentiation. The capacity to map splicing networks within complex tissues promises to uncover new disease mechanisms and biomarkers for cancer and other splicing-related disorders.
|
Myelodysplastic syndromes (MDS) are a group of cancers involving the blood and bone marrow. Specifically, MDS is considered a type of myeloid neoplasm. More details on how MDS is classified:
MDS is classified as a hematologic cancer arising from myeloid progenitor cells in the bone marrow, considered pre-leukemic in nature, and involving clonal expansion of genetically abnormal stem cells. Identifying it as a myeloid neoplasm is the most accurate terminology. |
Myelodysplastic Syndrome
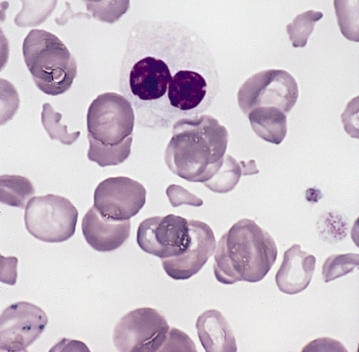
Myelodysplastic syndromes (MDS) are a group of blood cancers characterized by dysfunctional bone marrow that fails to produce healthy, mature blood cells. In MDS, immature blood cells known as blasts do not properly develop into mature red blood cells, white blood cells, or platelets.
The ineffective blood cell production in MDS leads to symptoms such as fatigue, shortness of breath, easy bleeding or bruising, frequent infections, and anemia. MDS has the potential to progress into acute myeloid leukemia in some cases.
MDS is more common in older adults, with an average age of diagnosis around 70 years old. The exact causes are not known, but risk factors include previous chemotherapy or radiation therapy, exposure to chemicals like tobacco smoke or pesticides, and heavy metal exposure.
Diagnosis of MDS involves examining blood cell counts and the percentage of blasts in the bone marrow. MDS is classified into different subtypes based on the types of cell lines affected and specific cytogenetic abnormalities.
Treatment options for MDS include blood transfusions, growth factors, chemotherapy drugs like azacitidine, and stem cell transplants in some cases. The prognosis varies depending on the MDS subtype and blast percentage. Overall survival averages around 2-3 years after diagnosis.
First recognized in the early 1900s, MDS was termed “myelodysplastic syndrome” in 1976 to describe this group of blood disorders with dysfunctional bone marrow and blood cell production. MDS remains an active area of cancer research given its heterogeneous nature and risk of progression to leukemia.
|
Here is some background on the etymology of the term “myelodysplastic syndrome”:
So “myelodysplastic syndrome” literally translates to a pathological syndrome characterized by faulty or difficult formation of blood cells in the bone marrow. The key roots are:
Putting these together into “myelodysplastic” captures the dysfunctional blood cell development in the marrow that defines these disorders. Adding “syndrome” signifies its recognition as a medical syndrome with a common underlying cause. The term myelodysplastic syndrome was first used in 1976 to unify several previously described disorders including refractory anemia and preleukemia under one umbrella terminology. The name succinctly captures the marrow abnormalities central to this condition. |
Abnormal RNA splicing is being increasingly recognized as a driver of many human diseases, including cancer. A new study led by researchers at Weill Cornell Medicine demonstrates the utility of analyzing RNA splicing patterns at the single cell level to understand how mutations lead to disease.
Using an enhanced technique called GoT-Splice, the researchers analyzed individual bone marrow cells from patients with myelodysplastic syndrome (MDS) caused by mutations in the splicing factor SF3B1. MDS is a blood cancer characterized by dysfunctional bone marrow and inefficient blood cell production. The single cell analysis provided unprecedented insight into how the SF3B1 mutation disrupts normal RNA splicing and cell maturation, leading to the ineffective hematopoiesis that defines MDS.
Specifically, the SF3B1 mutation was found to alter splicing and expression of genes involved in cell survival, maturation, and other key pathways. This shifted cell development towards the red blood cell lineage and allowed abnormal cells to proliferate, explaining the clinical picture of MDS. These findings identify new therapeutic targets and demonstrate the power of single cell multi-omics in connecting splicing alterations to disease phenotypes. More broadly, this work establishes a promising approach to map splicing networks in cancer and other splicing-related diseases at a precise single cell level.
This study demonstrates the utility of single cell multi-omic analysis of RNA splicing in elucidating mechanisms of splicing-related diseases like MDS. The findings provide specific insight into how SF3B1 mutations promote MDS while also establishing a broadly applicable tool to examine splicing programs driving disease development and progression.
Elucidating Splicing-Related Disease Mechanisms and Biomarkers
The researchers emphasize that GoT-Splice provides a versatile new tool for connecting aberrant splicing programs to disease phenotypes in any tissue of interest. By profiling splicing networks at single cell resolution, this approach can uncover new mechanisms by which splicing factor mutations drive pathology in cancer and other disorders.
In the future, single cell splicing analysis may identify new biomarkers associated with high risk disease subtypes or predictive of therapeutic response. As the researchers suggest, GoT-Splice could also detect precursor stages of overt disease, as they observed MDS-like splicing changes in patients with clonal hematopoiesis.
More work is needed to fully characterize the functional effects of splicing alterations on cell behavior across differentiation trajectories in development and disease. But this study exemplifies the insights that can be gained from single cell multi-omic assessment of the splicing landscape within complex, heterogeneous tissues.
Understanding the specific splicing disruptions underlying human diseases will open new possibilities for targeted therapies. The researchers note the discovery of BAX splicing alterations as a potential resistance mechanism for the drug venetoclax in MDS. Overall, this work establishes an exciting approach to decode how splicing factor mutations drive pathology, uncovering new prognostic markers and therapeutic opportunities.
Diseases that are similar or related to myelodysplastic syndromes (MDS)
- Acute myeloid leukemia (AML) – A rapidly progressing blood cancer that also originates in the bone marrow. Some cases of MDS can transform into AML.
- Myeloproliferative neoplasms – A group of bone marrow cancers that leads to overproduction of abnormal white blood cells, red blood cells, or platelets. Includes polycythemia vera, essential thrombocythemia, and myelofibrosis.
- Aplastic anemia – A condition where the bone marrow fails to produce enough blood cells, leading to low counts. It has a different cause than MDS but similar symptoms.
- Paroxysmal nocturnal hemoglobinuria (PNH) – A rare blood disorder also characterized by abnormal blood cell production and destruction, caused by a genetic mutation affecting red blood cells.
- Pure red cell aplasia – A disorder specifically affecting red blood cell production, leading to severe anemia. Can have some overlapping causes with MDS.
- Myelofibrosis – A type of myeloproliferative neoplasm that causes fibrous scar tissue to build up in the bone marrow, impairing blood cell production.
- Leukemias – Blood cancers arising from white blood cells. Chronic myeloid leukemia and hairy cell leukemia have some similarities in symptoms and bone marrow abnormalities to MDS.
- Lymphomas – Cancers originating from lymphocytes. Some types like T-cell prolymphocytic leukemia can resemble MDS under the microscope.
Treatments:
Here are some of the most promising treatments and potential cures currently being explored for myelodysplastic syndromes (MDS):
- Hypomethylating agents – Drugs like azacitidine and decitabine that can reactivate gene expression and restore normal function in MDS cells. They have improved survival for some patients.
- Immunomodulatory drugs – Medications like lenalidomide that modify the immune system and have shown efficacy in low-risk MDS patients.
- Luspatercept – A new drug that stimulates maturation of red blood cell precursors and reduces transfusion dependence. Recently approved for MDS treatment.
- Splicing modulators – Compounds that target splicing abnormalities in MDS are in early clinical trials, with some positive initial results.
- BCL2 inhibitors – Drugs like venetoclax that target anti-apoptotic proteins may enhance cell death in MDS.
- HDAC inhibitors – Epigenetic modulating agents that may help reactivate genes abnormally silenced in MDS.
- Bone marrow transplant – The only current proven cure for MDS is allogeneic stem cell transplant, though this intensive treatment has limitations.
- CAR T-cell therapy – Early research on reprogramming T-cells to target MDS blasts.
- Gene editing – Gene editing tools like CRISPR are being studied as ways to directly correct splicing factor mutations underlying MDS.
While still an incurable disease, progress is being made on targeted therapies tailored to the specific molecular defects driving MDS subtypes. Allogeneic stem cell transplant remains the gold standard for cure, but newer options continue to emerge to prolong life and quality of life for MDS patients.
Citation:
Image Credit: Public Domain – https://commons.wikimedia.org/wiki/File:Hypogranular_neutrophil_with_a_pseudo-Pelger-Huet_nucleus_in_MDS.jpg